Vishal Argawal, co-founder and Chief Product Officer of “Care Cognitics,” appeared on HCBiz show, a podcast dedicated to unraveling the business of healthcare. He was interviewed by host Don Lee in Lee’s final onsite interview at the HITExpo in New Orleans. Here is their conversation about Care Cognitics’ relationship to the gambling industry and new technologies that align provider and patient needs, lightly edited for clarity:
Vishal: Hey! Thank you so much for having me.
Don: So, I’m going to give you a wide opening starting point, sort of… Could you just tell the audience what does Carecognitics does, and who they do it for??
Vishal: Yeah, so at CareCognitics, we are applying concepts from industries outside of the healthcare sphere, such as the casino industry, in particular their loyalty concepts and gaming technologies, to help save lives–and to enable chronically-ill patients to lead a healthier life.
Don: Ok, interesting. That’s obviously a complaint that we hear coming up a lot, that healthcare needs to look to other industries or solutions to the problems that we are facing internally. I haven’t heard of anybody coming in from the casino industry, so this is a first for me. So, what can the casino industries’ loyalty programs teach healthcare?
Vishal: Well, let me give you an example: While working in the casino industry, we realized that I can fly someone a thousand miles, get them to Vegas, have them lose money, and have them still return home happy and wanting to come back to Vegas again. So, if I can do that for the casino industry, then why, in health care, can’t we get someone to show up at their doctor’s office for a free annual healthcare visit, which is actually good for them? That was the question we were asking ourselves. Or to look at another industry,
If Amazon can send me an alert today that says, “Hey, your dishwasher is going to run out of liquid in five days,” why can’t I get an alert from my doctor that says, “Hey there’s something wrong with your health, you should come and check it out”
or something like that? Or, you know what? Did you ever miss a flight?
Don: Yes, of course I have.
Vishal: So, looking at the airline industry… Could you imagine if Southwest never sent you an alert that your flight running late, and you showed up at the gate, and the flight was several hours delayed? What would your reaction be?
Don: I would not be very happy. And,, I think there would be a lot of angry people at the gate there with me too.
Vishal: Yeah? Well, when was the last time you went to the doctor’s office?
Don: Oh, I’ve had bad experiences waiting at the doctor’s office, for sure.
Vishal: Were there angry people out there?
Don: Yeah, everyone tends to look pretty harried when you get into a doctor’s office waiting room.
Vishal: Has that changed, ever?
Don: No…
Don: Yeah, everyone tends to look pretty harried when you get into a doctor’s office waiting room.
Vishal: No. Why?
Don:
As patients, we don’t have a lot of options. If we need care, we kind of get to a point where we kind of have to get it the way we can, and sometimes this is the only way it’s available.
Vishal: Yeah. Right. So, as patients, we are at the mercy of healthcare.
Don: Exactly.
Vishal: I think that has to change. Every other industry has changed. We forced the change. People forced the change. The technology is there; if Southwest can send us and alert that says, you know what, your flight is four hours late, then why can’t we get a similar alert from a physician’s office? I’m pointing out each of these things coming from an outside industry. We solve for a lot of these problems in the context of a casino. And what is very interesting to us is that the population that goes to casinos–especially in markets like New Orleans, which are outside of gaming centers like Vegas–has an average age of 52 years. Fifty-two years old, and very digitally savvy. They all have their loyalty cards, they are playing and engaged. So, the profile is of the average casino goer is similar to the average consumer in the Medicare healthcare space.
Don: I was going to ask you if you know what that average age is. Fifty-two is probably pretty close to average I would think, right?
Vishal: Yeah, especially once you leave the destination markets like Vegas and Atlantic city. If you leave those aside and look at the frequency market, as we call it, atthose casinos, the average age is pretty high. The local people coming there love to game and gamble, and they’re an older population. And, just like in healthcare, everyone is subject to luck–which you can’t change. But, casinos have very sophisticated technology. When you walk into a casino, they know, “Don loses maximum 100 dollars a day.”
Don: Right.
Vishal: And if we detect that Don just lost 300 dollars, you would think that we are happy. The casino should be happy: “Hey, we made more money!”
Don: But you’re probably worried that I’m unhappy, because now I’m not going to come back and lose 100 bucks three more times.
Vishal: Exactly! You’re going to say, “This is an unlucky casino.” And from the casino’s viewpoint, that’s not good. That means I’ve lost you, Don.
Don: That’s interesting. I’ve never thought of it that way.
Vishal: I can’t afford to lose you, right? So, what we do through casino loyalty programs to address this in real time–not five days later, nor five months later–we see, “Oh man, Don just lost 200 dollars more. He’s probably feeling unlucky.” And someone will pop up to you and say, “Hey it’s your lucky day.” We give you a free show ticket that’s probably worth 200 dollars or more (and that, in any case, would otherwise have had empty seats.) So, we’ve just switched your experience. I can’t change your luck, but I at least made your experience pleasant. Now you’re thinking, “Well, I lost 200 dollars, but I got 300 dollars of value. Maybe it’s still my good day–still my lucky day.”
Don: So, how do you take a concept like that and take it into healthcare? Because, you know, I can compare and contrast the experience here: If I’m going to gamble, it’s because I enjoy it, and it’s this fun thing, and there’s some risk and the potential for reward, and there’s all the things that we like as people, right? But there is almost nothing I like about going to the doctor. So, you are starting in a different spot. So how do you take that–you know those concepts–and apply them in a healthcare setting, which is a situation wherein I’m going somewhere that I wish I didn’t have to go to.
Vishal: Yeah, you’re right. What we are doing is this: Just like how in the casino, I can’t change your luck, but I can change your experience. We are focusing on chronic conditions.
When it comes to chronic conditions, even a physician cannot change your chronic condition.
They can only best manage it for you. Like, if you’re a diabetic, unfortunately, you can manage it, but you can’t cure it. It’s lifelong. People come to a casino to have fun but why would they go to the doctors office? Can healthy behavior be just as positive as a casino? So just like I cannot change your luck, I cannot change your medical conditions–but at least I can make your experience more pleasant, so there isn’t a barrier to care. You hate going to the doctor partly because the experience is so poor. Do you like to wait on a phone call for at least 5 minutes before you get to the front desk for your doctor’s office? Then you have to wait until you and COME IN to have any resolution? Can you imagine if you called up Comcast or AT&T and you had to wait for as long as the doctor’s office to have help? You would be pissed. We are not used to quick resolution and the convenience we expect in other industries for the physician’s office. Ironically, this is perhaps a situation where it is even more important to reach someone and have help quickly. It is more important to treat or manage illness than get your cable turned back on. So, we are bringing in the concierge services that you are used to in an entertainment environment, like a casino, and applying them to healthcare. So, through the physician practices and providers that sign up for our service and make it available to their patients, we offer and manage concierge services to people–to those providers–so that their patients can actually call us. We offer same day appointments; we offer 7-by-24 service. We learned that from the casino industry.
Don: So how are you providing those services? You are providing access to those services for your customers who are the doctors, or do you also have clinicians that are part of your team?
Vishal: What we do is this: Our customers are the physician practices. We offer our service to the physician practice, and for the physician practice we offer in-between office visit care for chronic patients. Chronic patients are where the cost is the highest and they need the most care. And most of their problems happen in between office visits. That’s when things go wrong. We provide a service that is a combination of a technology platform and a medical assistant team that we have on our staff.
Don: These people on your team answer questions and do the little check-ins in between and stuff like that?
Vishal: Yes. 100%. Physicians sign up and our team manages the services and patients can sign up. And where our loyalty concepts come in from casino is that we offer incentives to the patients to make healthy choices, right? These incentives are very carefully crafted. You know if you offer a free gym membership to someone who is obese,chances are they are not going to use it much. But that’s what we see in healthcare–it’s a “spray and pray” approach. It is not customized.“Hey, let’s give this benefit to everybody.” Guess who ends up using those gym benefits? People who are already fit.
Don: Yeah, what’s funny is–not to go off on a tangent–but that health plan that offers a free membership is designed so the people who go to the gym self-select into that plan. They are actually building a plan for healthy people.
Vishal: Exactly. That’s always been the case. The people who aren’t already inclined to go to the gym need different types of incentives. They need incentives that they value. In a casino, what we realized very quickly was that the best incentive costs to the casino zero dollars. Do you know what that was? To be told happy birthday on their birthdays.
Don: Oh yeah, people love that. People love to be recognized.
Vishal: That’s it–and, it didn’t cost anything. It wasn’t, you know, a free coupon to a buffet.
Don: So, I love the concept. What is something–I mean I guess they could just say happy birthday–but what is an example that is applicable in the doctor’s office that you recommend to your people?
Vishal: Same day appointments.
Don: Same day appointments? Okay, so how do you get the doctors to do that–like they are going to have to keep space in their schedule?
Vishal: Yeah–you’re totally right. They keep designated space in their schedule.
Don: So that’s got to be a big leap for a lot of them;not to fault doctors, but it’s like the system is kind of designed to grind them into these 15-minute appointments, which itself makes clients wait in the waiting room so that there aren’t any gaps. Everything is kind of stacked against the patients and the doctors in this scenario, so how do you get the doctors to create space in their schedules?
Vishal: So, there’s a two part answer, right? One, when we offer this service for the providers, we actually don’t charge physicians any money. We piggyback on a Medicare program for chronic conditions which allows for reimbursement of great care; it’s a chronic care program that offers incentives to the physicians. So, through our service, we are not only able to facilitate better care for their patients; we also make money for the provider’s office. They are already providing the care and able to meet requirements for treating chronic conditions. I think it’s the best alignment that we’ve seen. So that’s the business model that we follow.
In terms of offering these incentives to the patients, even in the casinos, not everybody gets all the benefits. People who have the need get those benefits. So, we “right size” these benefits to people who are really in need.
The example that I gave you: even though that is a base benefit, we ask the physicians to create some space for the patients who sign up in this program. The physician’s office doesn’t have to do any additional work. We do that work for them. We manage their patients. We do things on their behalf, but in return we do ask of some things from the doctors to enable this–and that includes, if one of our MA’s calls in and says, “You know we need you to see this patient,” then they make time for that patient. Many a time, there’s a human touch that is missing because everyone is so burnt out. With our system, if we can’t get the same day appointment, we call back the patient and say, “Hey I’m sorry, I can’t give you that today, but it’s available tomorrow, all right?” Nine times out of 10, they are fine with that.
Don: I would be thrilled if I could see my doctor tomorrow.
Vishal: Yeah, but just getting a call that saved you the trouble of waiting 5 minutes to speak to a doctor, just to get to a receptionist who says, “Yeah please come in four weeks”—it’s just a very broken experience that we’re trying to improve upon.
Don: I just had an experience where I had to wait two months. I’m not a chronic patient–I’m going for like my routine checkup–but I’m waiting 2-2.5 months to get my appointment. Which is madness.
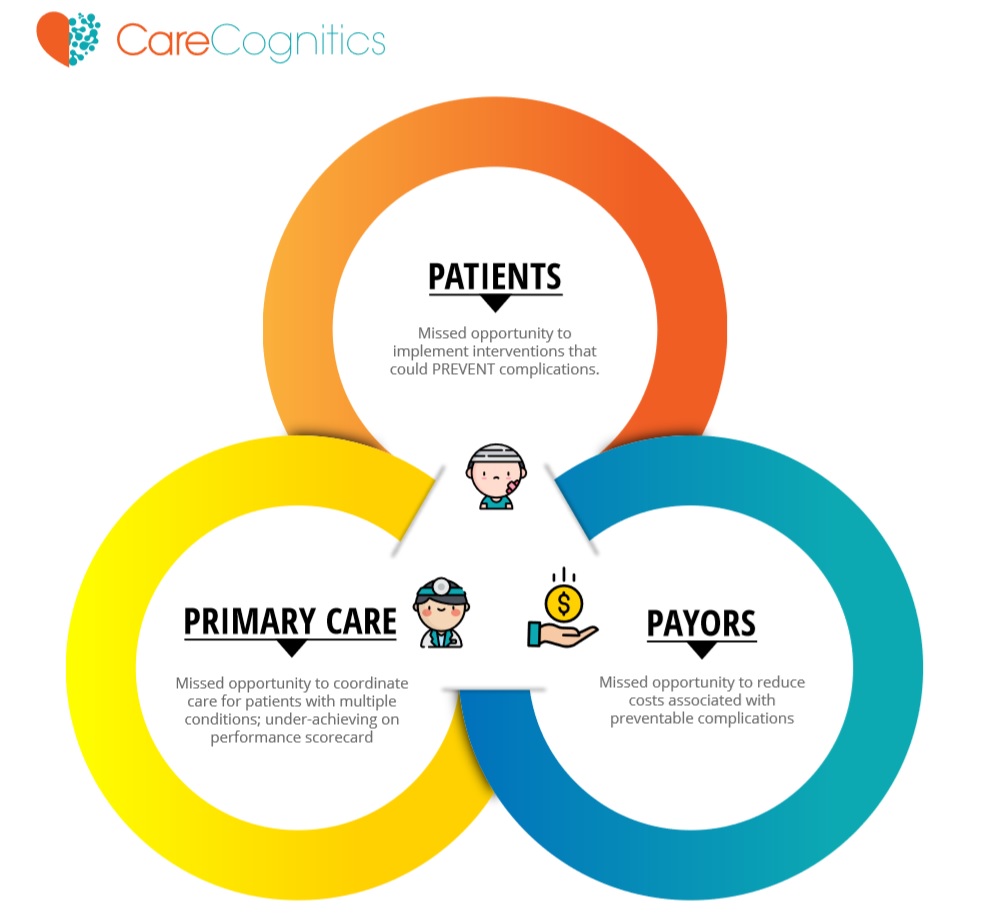
Vishal: Exactly- and we are not in the business of fixing everything. We can’t be. But we do think that as a company we can make a difference, both in terms of our business model that aligns incentives between the physicians and patients, and the physician benefits that are gained, because we are helping them increase their revenue. And the patients definitely benefit from it because they’ve got a personal concierge who is looking out for them every month, seeing what their needs are and reminding them of things. And in the process, there’s a reason why we’ve seen great adoption from our patients; we’ve broken MIPS and 78-year-olds are engaging with us digitally, which we didn’t think would ever happen.
People want to be in the program because it is based on their personal needs and improves their health care experience. Physicians want to be part of it because we are not adding additional overhead or work for their staff or for themselves.
I think this is a great program for Medicare, and I think it’s driving great alignment for us. It is about organization since you already see those patients, but this way the physician practice is proactive about their care rather than reacting with bad scheduling delays.
Don: Yeah, I love how you tied the concierge approach on top of the chronic care management and the Medicare code because you’re not funded. It would have been, I imagine, a very difficult sale to go into a doctor’s office and say,“Hey, you’re going to pay us to go and offer this concierge service on your behalf, and oh, by the way, you’ve got to create a gap in your schedule every day because we are going to be sending you same day appointments–cool?” I don’t think that would have worked. So the face that you were able to piggy back that onto the 99490…there was already some demand being created. Physicians are already aware of this; they want to take advantage. I love the business model of basically saying, “Doctor, you don’t have to do much other than coordinate with us and agree to let us come in on your behalf.” You’ve got to create trust.
Vishal: Exactly.
Don: And once they trust you–the barrier to them starting off with this service to their patients is pretty low. Right? Am I missing something?
Vishal: No, I think that is exactly right and I think you know we’ve designed our service to be exceptionally patient-centric. Everything that we do and bringing incentives onboard–you know, providing care–we didn’t have to do any of that. But we are doing that because at the end of the day what we believe is that showing value every month to those patients are critical. There is a copay involved in this right? And even though it’s a low copay, it’s still eight to ten dollars. That’s the cost of a Netflix subscription. We consider it that way. We are competing for that 10 dollars that you may use to sign up for a Netflix so that you can be entertained every minute of the day. Can I show you enough value to stay in this program? Because it’s not just about sign up and getting the patient enrolled. It’s about getting patients to feel that, month after month, the program is really helping them.
Don: Yeah, it’s about getting them to keep spending that 8 bucks every month–and to a lot of people listening, I’m sure that doesn’t sound like very much money, but to some people that’s actually a question that they ask themselves every month, particularly those who already have an expensive chronic condition.
Vishal: Absolutely, they do.
Don: It’s like,do I want to redirect those funds to gas for my car, or is this still worth it? So yeah- that’s important.
Vishal: And we believe that:
For the population that we work with–health is important. For the Medicare population, health is a top priority. And we believe that strengthening that relationship with their primary care is the right thing to do.
There’s already trust in that relationship. It’s just that as you said at the start of the podcast–we don’t think of our physicians until we really are sick. And if we want to turn the tide of rising healthcare costs and improving the life of our members, that has to change. We feel that the change starts by strengthening that physician-patient relationship by removing barriers, by making it more personal, by making it more timely, and making it more rewarding for the patients. Incentivizing them with the right things. It’s really those 4 things that we are offering through our service and hoping that we will be able to make a meaningful difference.
Don: No, it sounds great. Now how long have you guys been at it for?
Vishal: We launched our service last March. So, it’s fairly new but we’ve got good traction. We’ve got about 2000 active patients on the platform in 4 states. We’ve got a pool of about 20,000 more Medicare patients that we are in the process of signing up.
Don: Awesome. And do you have any particular success stories you can point to? Even if it’s anecdotal, like a story you heard about this one patient. What can you share about what is happening?
Vishal: Yeah, last week one of our medical assistants just dropped a note on our internal communication channel, telling us that one of the patients had said, “Oh my God, if that’s the kind of service I’m going to get, I’m going to get my husband to sign up with this program too.”
Don: Oh, there you go. That’s your net promoter score right there, right?
Vishal: Yeah, and you know, that’s great! You know it’s awesome. But again–there is also the other side. People who have dropped out of the program. And they’ve dropped out of the program because they didn’t get full participation from the providers.
Don: So, you basically weren’t able to deliver the whole service in that scenario, I imagine.
Vishal: Yeah because as much as we take the burden off of the providers, this is still a partnership. At the end of the day, we are coordinating care. We are not providing care. The providing of care still happens at the provider side. If we want this person to come in because we’ve detected that this person is at risk, but if the physician’s office didn’t make space, or didn’t follow through for some of our care coordination, then the system breaks. So, what we are learning very quickly is that there is a profile of providers that work better with us and a profile of providers who don’t work as well with us.
Don: Are you going to have to be really picky about who you work with? Because otherwise, if someone signs up but there is no follow-through, then it will make you look bad.
Vishal: Exactly. So as we grow as a company, that’s our learning. Trying to see who we partner with on the provider side–who is going to really make at least some level of changes, so that when we have a recommendation for a certain patient, or if we say, “Hey, this patient needs to come in tomorrow,” you know we get that support from them.
Don: That makes sense. Awesome. Lastly, where can people go to learn more about you guys?
Vishal: You can learn about us from https://carecognitics.com/. You can even follow us on Twitter–and please drop us a note. We are looking to partner with family practices from about 5 primary care physicians to about 99. Again, our services don’t cost anything to the providers–we help them raise their revenue while providing coordinated care for their chronic patients.
Don: Awesome. I’ll add that, so you guys can find that nice and easy, and that’s it. Vishal, thank you so much for spending the time today–it’s really fascinating stuff.
Vishal: Thanks, Don.
You can listen to the episode HERE.
Are you a physician’s practice that wants to meet with our team? Please CONTACT US HERE.