ANNUAL WELLNESS VISIT: OPPORTUNITY LOST TIMES 3?

ANNUAL WELLNESS VISIT: OPPORTUNITY LOST TIMES 3?
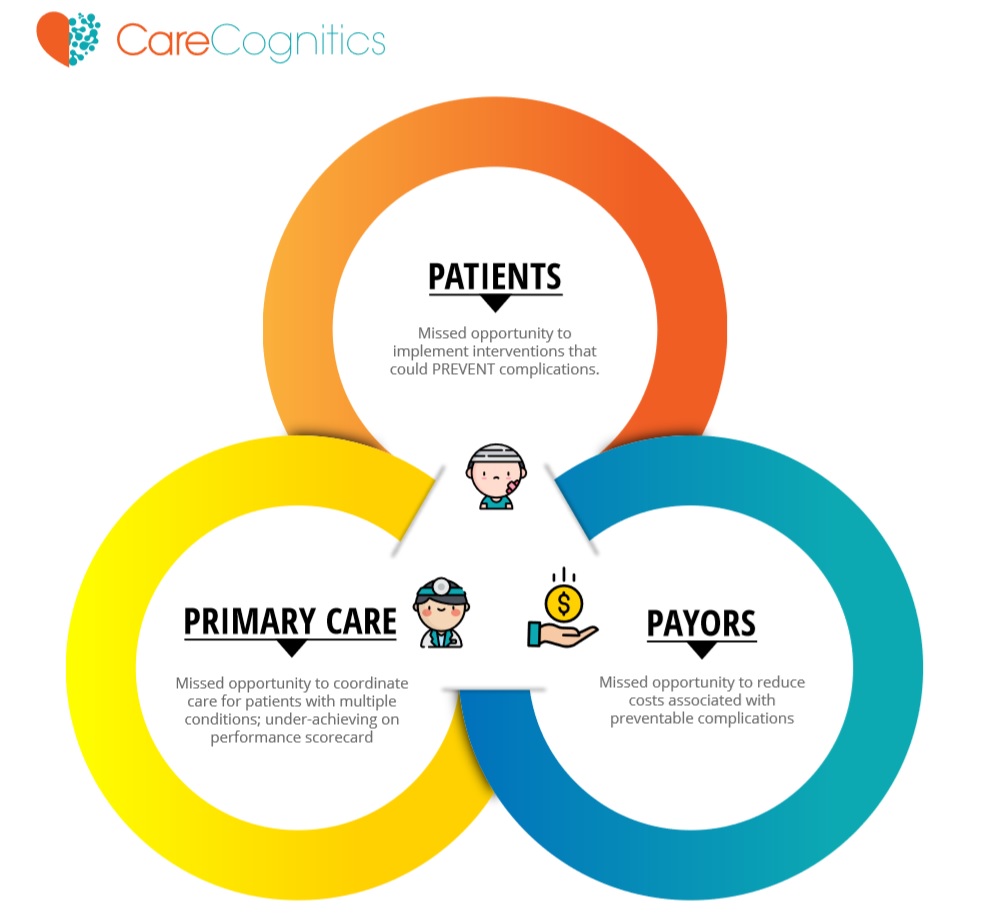
For Patients:
Missed opportunity to implement interventions that could PREVENT complications
For Primary Care:
Missed opportunity to coordinate care for patients with multiple conditions; under-achieving on a performance scorecard
For Payors:
Missed opportunity to reduce costs associated with preventable complications
The concept of the annual wellness visit is the classic “no-brainer” – one of the rare instances in which a concept is favorably received by all parties without any negative consequences.
What’s not to like?
- Patients like the comprehensive review of their medical problems including all the measures necessary to improve their condition. As such, the Annual Wellness visit also represents an opportunity to mitigate the “fragmentation” of medical care that is associated with multiple providers.
- Primary care physicians like the extended time that helps to coordinate and prioritize all the health measures and help to ensure that their interventions are compatible and non-duplicative. As such, the Annual Wellness Visit is the antidote to the typical clinic visit which by necessity is focused on one problem. Moreover, reimbursement levels are commensurate with the extended time in the office.
- For Payors, the comprehensive assessment is the best chance to create an intentional, coordinated, and pro-active game plan for the patient that has the chance to PREVENT complications and hospitalizations.
I regularly review Annual Wellness Visit reports from primary care physicians – the notes are beautifully constructed and provide a comprehensive assessment of the patient along with recommendations to help improve outcomes of the different disease states.
BUT, what typically happens next is that the summary gets filed and the lack of progress is noted on the next follow-up visit.
With all these positives, why does the Annual Wellness Visit break down? Why doesn’t the Annual Wellness Visit lead to the better outcomes that it was designed to produce?
In my opinion, the most important reason is the lack of a system to help the patient implement the action plan. We expect patients to implement the action plan but they need coaches. Doctors are not coaches and should not be expected to be coaches.
The typical Medicare patient is given a paper or electronic summary of all the measures that need to be actuated – the information is simply overwhelming for the patient with multiple chronic diseases. How does the typical patient increase the intake of fruits and vegetables, exercise three times a week, lose weight, stop smoking, get a screening mammogram/colonoscopy/bone density scan, monitor blood pressure, take all medications, and get a flu shot in the Fall?
But what if there was a SYSTEM to help the patient implement the recommendations, in the correct priority, in a fashion that was tolerable, sustainable, and scalable? What if we had a system and a coach who could help walk the patient through the implementation of the plans that are outlined by the Annual Wellness Visit? Here are some ideas of what the system could look like:
- An electronic communication platform so that the patient can communicate with the primary care office without depending on the telephone.
- An automated system that helps the patient implement the care plan, as directed by the primary care physician, in the correct sequence.
- Primary care offices should be automatically notified if there are lapses in the communication or if plans are not being implemented.
- Patients are sent regular reminders and follow-up messages that serve to reinforce and encourage the correct behaviors.
- Patients can identify key members (family and friends) who can help the patient – these key members should be included in all communications.
I believe that such a system could transform the Annual Wellness Visit from a “one and done” visit to the start of the comprehensive health plan that it was designed to be!

Click to View the Full Size 5 Points InfoGraphic

